 The ICD-10 transition has been smoother than many have expected. Although coder productivity is predictably down as technicians adjust to the new standards, denials have stayed virtually constant. Here is a look at the first month under the new ICD-10 coding standard from the Centers for Medicare and Medicaid Services:
The ICD-10 transition has been smoother than many have expected. Although coder productivity is predictably down as technicians adjust to the new standards, denials have stayed virtually constant. Here is a look at the first month under the new ICD-10 coding standard from the Centers for Medicare and Medicaid Services:
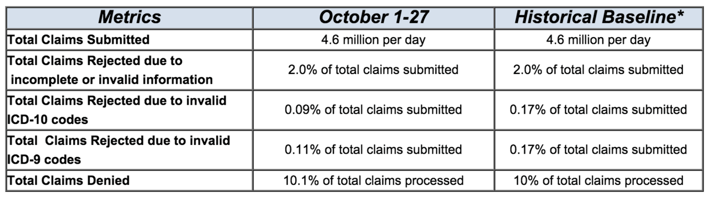 Chart from CMS.gov
Chart from CMS.gov
Total claims denied on account of invalid ICD-10 codes was only 0.09% of those submitted...less than one tenth of one percent! But before we get too excited about the low denial rates, it’s important to look at some of the reasons behind the numbers. Much of the mild result thus far is thought to be a consequence of the transitional rules CMS has put in place to ease the change. Here are three big features of the first year transition period that are making life easier until October 2017:
- The Centers for Medicare & Medicaid Services (CMS) are allowing physicians to receive advance payments in the event that ICD-10 issues are causing contractors not to process claims.
- For the first year, so long as claims are submitted in the appropriate family of ICD-10 codes, Medicare will not deny them.
- Submitting claims using the correct family of codes is also enough to avoid penalties for the next year (until October 2017) under CMS program features like meaningful use, the Physician Quality Reporting System, and value-based payment modifiers.
While these three initiatives will help private medical practices avoid painful denials for a while, they unfortunately only apply to claims filed through Medicare and Medicaid. Private insurers may or may not extend the same services, and depending on where the bulk of your patients are insured, the ICD-10 transition might be more difficult financially and timewise.
What to Expect Moving Forward With the ICD-10 Transition?
Although initial denial rates are minimal as shown above, that may not remain the case...especially after the grace period is over. Elizabeth Woodcock of Woodcock & Associates warns about “denial creep,” saying: “My concern is that right now payers are adjudicating pretty much everything that makes sense. When they start tightening up in the next 9-18 months, then we'll start to feel the squeeze.” She believes that pre-authorizations and pre-certification requirements will be affected first.
So what’s a private medical practice to do?
First, ensure that your practice maintains as much of a financial cushion as possible to ward off financial impacts of future denials. Second, make sure to address coder productivity when appropriate. It’s understandable to have some drop in productivity initially, but as the months tick by, errors should decrease and efficiency should increase. Third, make sure your practice has a solid process in place to track claim denials and follow up quickly and regularly. Great practice management software can help with this, and so can a great medical billing company.
It’s a few months into the transition and generally, it seems like things are going well. If that’s not the case for your practice, consider giving Keystone Health Partners a call to discuss how we can help you succeed. Thanks for reading!



